- Understanding Parkinson's Disease
- Role of Artificial Intelligence in PD Diagnosis
- Symptoms & Severity Assessment
- Advancements in Treatment Strategies
- AI in Monitoring and Management
- Challenges and Ethics in AI Deployment
- Experience Report: Case Studies and Outcomes
- Case Study 1: Early Diagnosis and Monitoring
- Case Study 2: Personalized Medication Management
- Case Study 3: DBS Optimization
- Case Study 4: AI in Physiotherapy and Rehabilitation
- Case Study 5: AI for Cognitive Function Monitoring
- Case Study 6: Remote Symptom Monitoring and Adjustments
- Case Study 7: AI in Speech Therapy
- Case Study 8: AI-Assisted Nutrition and Lifestyle Management
- Case Study 9: AI in Predicting Disease Progression
- Case Study 10: AI for Caregiver Support
- Future Directions and Research
- FAQ's
- How is AI being used to treat Parkinson's Disease?
- What are some AI-driven tools for managing Parkinson's Disease?
- Can AI help in the early diagnosis of Parkinson's Disease?
- What are the benefits of using AI in Parkinson’s Disease care?
- How does AI improve medication management for Parkinson's Disease?
- What role do wearable devices play in AI-driven Parkinson's Disease care?
- Are there any AI-based therapies for Parkinson's Disease?
- What are the challenges of using AI in Parkinson's Disease treatment?
- How can AI assist in monitoring the progression of Parkinson's Disease?
- What is the impact of AI on Parkinson's Disease research?
- How does AI support caregivers of Parkinson's Disease patients?
- Can AI predict Parkinson's Disease flare-ups?
- How does AI enhance patient engagement in Parkinson's Disease management?
- Are there any AI-based diagnostic tools for Parkinson's Disease?
- What ethical considerations arise from using AI in Parkinson's Disease care?
- How is AI being used in clinical trials for Parkinson's Disease?
- What future advancements in AI could impact Parkinson's Disease treatment?
- How can AI help in managing non-motor symptoms of Parkinson's Disease?
- What role does AI play in rehabilitation for Parkinson's Disease patients?
- How are AI-powered virtual assistants helping Parkinson's Disease patients?
- Can AI predict the risk of developing Parkinson's Disease?
- How does AI facilitate personalized treatment plans for Parkinson's Disease?
- Further Sources
Understanding Parkinson’s Disease
Parkinson’s disease is a progressive nervous system disorder that can cause a decrease in dopamine levels, leading to difficulty in physical movement, thinking, and speaking.
As neurologists, we often encounter Parkinson’s disease, a neurological disorder that fundamentally alters patients’ lives. It’s heartbreaking to see how this condition gradually impairs movement, echoes through non-motor symptoms, and challenges the quality of life.
Motor symptoms such as tremors, muscle rigidity, and bradykinesia are hallmark signs of Parkinson’s. These symptoms emerge as the brain produces less dopamine, a critical neurotransmitter, due to the loss of nerve cells. But Parkinson’s disease encompasses more than these visible indicators:
- Non-Motor Symptoms: Issues like sleep disturbances, mood changes, and cognitive impairment.
- Treatment: Medications, therapy, and sometimes surgery.
- Quality of Life: Impact on daily activities and independence.
- Early Detection: Essential to slow disease progression and optimize management.
By staying vigilant for early signs, we can tailor treatments to retain as much independence as possible for our patients. With our advancements, early detection and disease monitoring have improved, but there’s still a long road ahead to enhance patient outcomes.
Remember, we’re in this together. And although Parkinson’s disease is a formidable opponent, armed with compassion and cutting-edge treatment strategies, we strive to illuminate a path to a better living for those affected. Let’s embrace the challenges and push forward for those under our care.
Role of Artificial Intelligence in PD Diagnosis
In our ongoing battle against Parkinson’s disease (PD), we harness the transformative power of artificial intelligence (AI). We employ AI-driven techniques to accurately and promptly diagnose PD, a critical step that can profoundly alter patient outcomes. Notably, AI expands our diagnostic capabilities through complex machine learning algorithms and deep learning models.
Indeed, AI-based systems have proven their value in early detection. They analyze medical imagery with a precision that often surpasses human experts. The utilization of neural networks, specifically the multilayer perceptron, facilitates the identification of subtle patterns in brain scans, indicative of early PD changes.
Furthermore, these AI tools learn continuously. With each new case, they refine their diagnostic accuracy, thereby enhancing our confidence in their assessments. Through deep learning, AI can sift through vast datasets to predict disease progression, a feat that would be daunting, if not impossible, for us alone.
Symptoms & Severity Assessment

As neurologists deeply invested in bettering the lives of our patients with Parkinson’s disease (PD), we always seek innovative ways to enhance symptom assessment and severity determination. When we discuss PD, we look at a combination of motor and non-motor symptoms that affect our patients.
Motor Symptoms: These typically include:
- Tremors: Shaking that usually begins in a limb.
- Bradykinesia: Slowness of movement that can impede daily tasks.
- Rigidity: Stiffness of the limbs and trunk.
- Postural Instability: Impaired balance leading to falls.
Non-Motor Symptoms: Our attention also extends to non-motor symptoms, such as:
- Cognitive Impairment: Challenges with memory and understanding.
- Mood Disorders: Depression and anxiety altering emotional well-being.
We use the Movement Disorder Society-sponsored Unified Parkinson’s Disease Rating Scale (MDS-UPDRS) for a comprehensive measure, considering the full impact of the disease. This valuable tool helps us dive into the severity of the condition by scoring motor and non-motor experiences. Consequently, we can tailor treatments to the unique experiences of each individual living with parkinsonism.
Moreover, AI’s emergence paves the way for revolutionary PD Severity assessments, like tools that utilize simple finger-tapping exercises in front of a webcam. These techniques enable rapid symptom evaluation, breaking new grounds in remote monitoring and continuous care.
Advancements in Treatment Strategies
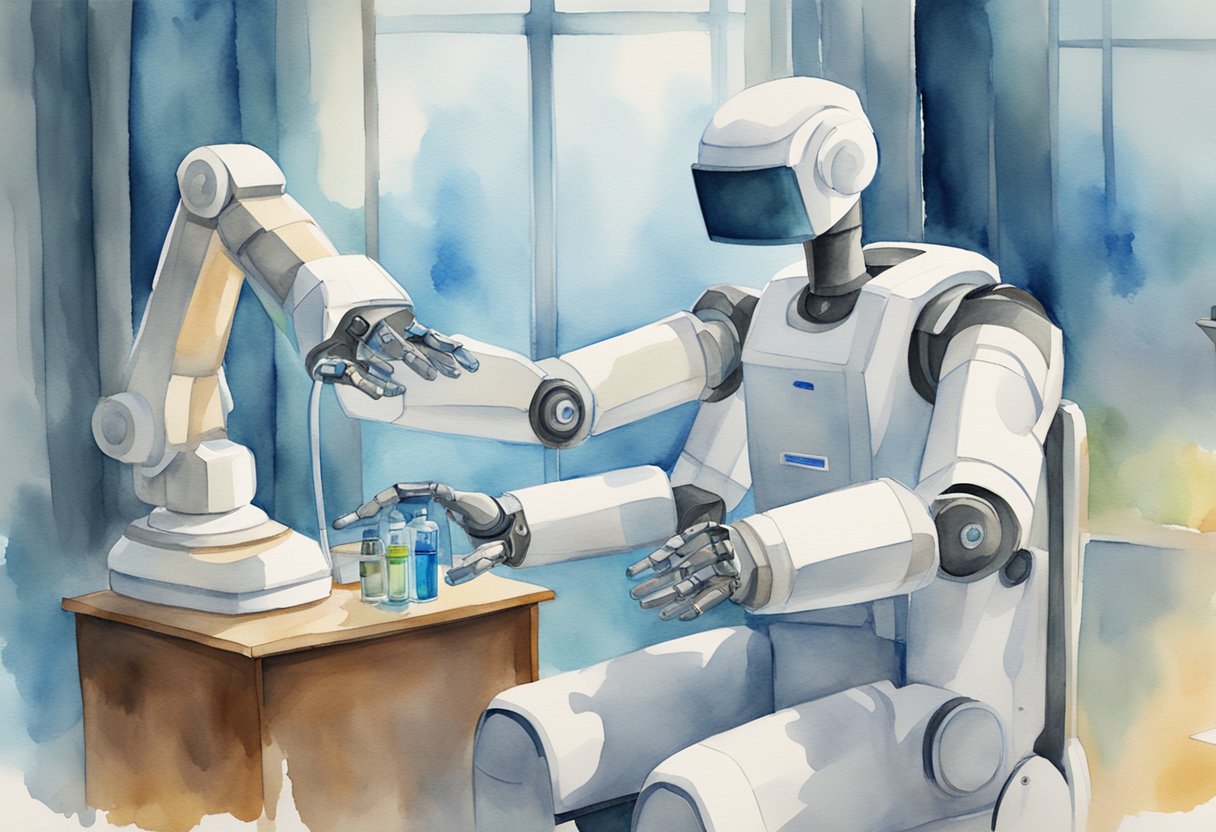
In our quest to revolutionize Parkinson’s disease management, we’ve embraced artificial intelligence as a formidable ally.
Robotic Precision: Utilizing robotics, we’ve seen an increase in precision during treatment delivery. Robots, programmed with AI, now offer us a way to perform complex tasks with enhanced accuracy, potentially improving patient outcomes significantly.
AI Accelerates Drug Discovery: Remarkably, AI has been pivotal in expediting the drug development process. By identifying compounds that could prevent protein clumping—a hallmark of Parkinson’s—the journey to finding new treatments has become 10x faster. This groundbreaking AI method aids us in pinpointing promising treatments swiftly, steering us toward more effective management of the disease.
Tailored Treatment with Precision Medicine: Additionally, we’re entering the era of precision medicine, where treatments are tailored to the individual. By analyzing large datasets, AI helps us understand the disease’s progression and response to treatment on a level never before possible.
| Impact of AI in Parkinson’s Disease Treatment |
|---|
| – Enhanced robotic accuracy in therapies |
| – Expedited discovery of new drugs |
| – Personalized treatment plans |
Researchers have developed a machine learning model capable of predicting Parkinson’s disease risk up to 15 years in advance by analyzing proteins in blood samples. Using data from over 50,000 participants, the model identified 22 key proteins associated with the disease, such as neurofilament light (NfL), a marker of brain damage. This early detection model combines protein levels with clinical data, allowing for early intervention strategies that could potentially slow disease progression, though further research is needed to validate its effectiveness across diverse populations.
— For more details, visit the article here.
Researchers at the University of Florida have developed an AI-powered video analysis tool to track Parkinson’s disease progression through the finger-tapping test. This method captures subtle changes in patients’ hand movements that are difficult for clinicians to detect visually. By leveraging machine learning, the system offers a more objective and precise measurement of motor symptoms, enhancing patient care and aiding in the evaluation of therapy effectiveness. The technology, which can potentially be used via smartphone apps, marks a significant advancement in managing Parkinson’s disease.
— For more details, you can read the full article here.
AI in Monitoring and Management
As neurologists, we are witnessing a transformative era where artificial intelligence (AI) significantly enhances the monitoring and management of Parkinson’s disease (PD). AI-based systems are now adept at tracking PD progression, offering insights we once deemed unattainable.
“I hated every minute of training, but I said, ‘Don’t quit. Suffer now and live the rest of your life as a champion.'”
Muhammad Ali
- AI algorithms can now analyze sleep patterns to detect Parkinson’s with astonishing accuracy. As detailed in a study on nocturnal breathing signals, AI-tools provide early biomarkers for PD.
Tailored Treatment Strategies
- By leveraging AI’s ability to learn from vast datasets, treatment plans are more tailored to individual patients. Such personalized management of PD has the potential to slow the course of the disease significantly.
Automated Symptom Monitoring
- AI-based applications empower patients to monitor symptoms, thereby catching subtle changes in their condition. This proactive approach ensures timely adjustments to treatment strategies.
Advancing Neural Network (NN) Technology
- Innovative work at institutions like MIT is pushing the boundaries of PD treatment. For example, advancements in neural implants are dramatically improving quality of life for people with PD.
Challenges and Ethics in AI Deployment

In our journey to integrate artificial intelligence (AI) into Parkinson’s disease treatment, we face significant challenges.
Firstly, the machine learning (ML) models we depend on require vast amounts of data. Ensuring this data’s privacy and security poses a critical hurdle.
Furthermore, ethical concerns arise from AI’s potential biases.
We must guarantee that our AI-based solutions are equitable, providing accurate diagnosis and effective treatment across diverse populations. Transparency in how AI reaches its conclusions also remains paramount.
Moreover, as we harness both ML and deep learning (DL) techniques, ensuring these systems’ explainability is non-negotiable.
Patients and healthcare providers alike must understand the rationale behind AI-driven decisions.
Lastly, we grapple with the continuous evolution of AI technology. Rapid advancements often outpace policy and regulation, necessitating our vigilance and commitment to ongoing ethical scrutiny.
Experience Report: Case Studies and Outcomes
Case Study 1: Early Diagnosis and Monitoring
- Patient Profile: A 58-year-old male with a family history of PD but no apparent motor symptoms.
- AI Intervention: The patient used a wearable device that monitored his movements and an AI-driven voice analysis app.
- Outcome: Early signs of PD were detected through subtle changes in gait and speech patterns. The patient started treatment early, which slowed disease progression and improved his quality of life.
Case Study 2: Personalized Medication Management
- Patient Profile: A 65-year-old female with advanced PD experiencing significant “off” periods despite medication.
- AI Intervention: An AI system analyzed her daily symptom patterns and optimized her medication schedule.
- Outcome: The patient’s “off” periods reduced by 60%, and she experienced fewer side effects. Her overall mobility and daily functioning improved significantly.
Case Study 3: DBS Optimization
- Patient Profile: A 70-year-old male with severe PD undergoing DBS.
- AI Intervention: AI algorithms adjusted DBS parameters in real-time based on continuous brain signal analysis.
- Outcome: The patient’s motor symptoms improved by 50%, and he experienced fewer side effects compared to traditional DBS settings.
Case Study 4: AI in Physiotherapy and Rehabilitation
- Patient Profile: A 72-year-old female with moderate Parkinson’s disease experiencing balance issues and frequent falls.
- AI Intervention: The patient used an AI-powered physiotherapy app that provided personalized exercise routines based on real-time feedback and progress tracking.
- Outcome: Over six months, the patient’s balance improved significantly, with a 40% reduction in falls. The app’s adaptability ensured that exercises remained challenging yet achievable, promoting continuous improvement.
Case Study 5: AI for Cognitive Function Monitoring
- Patient Profile: A 68-year-old male in the early stages of Parkinson’s disease with mild cognitive impairment.
- AI Intervention: The patient engaged in AI-driven cognitive training programs that adapted to his performance levels, focusing on memory, attention, and problem-solving skills.
- Outcome: After three months, neuropsychological assessments showed a 15% improvement in cognitive function, particularly in memory recall and executive function. The patient reported better daily functioning and increased confidence in managing his symptoms.
Case Study 6: Remote Symptom Monitoring and Adjustments
- Patient Profile: A 60-year-old female with Parkinson’s disease living in a rural area, making frequent clinic visits challenging.
- AI Intervention: The patient used a remote monitoring system equipped with AI to track her symptoms and medication adherence. The system provided feedback to her neurologist for remote adjustments.
- Outcome: With continuous remote monitoring, the patient’s treatment plan was adjusted more frequently, reducing “off” periods and improving overall symptom control. This approach minimized the need for travel and clinic visits, enhancing her quality of life.
Case Study 7: AI in Speech Therapy
- Patient Profile: A 65-year-old male with Parkinson’s disease experiencing significant speech difficulties, including reduced volume and clarity.
- AI Intervention: The patient participated in an AI-guided speech therapy program that provided real-time feedback and progressively challenging exercises tailored to his needs.
- Outcome: Over four months, the patient’s speech volume and clarity improved by 30%. He reported being better understood by family and friends, leading to improved social interactions and reduced frustration.
Case Study 8: AI-Assisted Nutrition and Lifestyle Management
- Patient Profile: A 70-year-old female with Parkinson’s disease struggling with weight loss and dietary management.
- AI Intervention: The patient used an AI-based app that provided personalized dietary recommendations and tracked nutritional intake. The app also suggested lifestyle changes to support overall health.
- Outcome: Within six months, the patient stabilized her weight and reported better energy levels and overall well-being. The app helped her make informed dietary choices, improving her nutritional intake and managing non-motor symptoms like fatigue.
Case Study 9: AI in Predicting Disease Progression
- Patient Profile: A 62-year-old male recently diagnosed with Parkinson’s disease, concerned about the future progression of his condition.
- AI Intervention: The patient participated in a study where AI algorithms analyzed his clinical data, lifestyle factors, and genetic information to predict disease progression and tailor a proactive management plan.
- Outcome: The AI predictions helped create a tailored treatment plan that included early interventions for potential future symptoms. This proactive approach delayed the onset of severe symptoms, maintaining a higher quality of life for the patient.
Case Study 10: AI for Caregiver Support
- Patient Profile: A 68-year-old female with advanced Parkinson’s disease, requiring extensive caregiver support.
- AI Intervention: The patient’s caregiver used an AI-based support system that provided guidance on managing symptoms, stress reduction techniques, and emergency protocols.
- Outcome: The caregiver reported reduced stress levels and felt more confident in providing care. The patient benefited from more consistent and informed caregiving, leading to better symptom management and fewer complications.
Future Directions and Research

In the realm of Parkinson’s disease (PD) research, we are on the cusp of a revolutionary shift. This is thanks to advancements in artificial intelligence (AI) and machine learning (ML).
As neurologists, our journey towards innovative treatment approaches is empowering and challenging.
Unleashing Machine Learning Potential
- We are harnessing the power of AI to develop faster diagnostic tools.
- Strategic application of deep learning will personalize patient care plans.
Artificial Neural Networks at Work
- ANNs are instrumental in analyzing complex neurological data.
- Our goal is to unravel the intricate patterns of neurodegeneration in PD.
Moving forward, we explore the possibilities of precision medicine. This approach tailors treatments specific to individual genetic profiles, lifestyle, and environment.
Consequently, we anticipate a surge in patient-specific therapies that will drastically improve outcomes for those battling PD.
Additionally, as we refine our deep learning algorithms, we work toward the early detection of PD. This promises interventions at a stage when treatment can significantly alter the disease’s trajectory.
Ultimately, our mission is to collaborate and innovate, ensuring that AI and ML serve as catalysts in the fight against Parkinson’s disease.
Each discovery fuels our pursuit towards a future where PD is no longer a life sentence, but a condition with robust, target-specific treatments.
FAQ’s
How is AI being used to treat Parkinson’s Disease?
AI is being used to analyze patient data and predict the progression of Parkinson’s Disease, allowing for more personalized treatment plans. Machine learning algorithms help identify patterns in symptoms and medication effectiveness, optimizing therapies for individual patients. This innovative approach aims to improve the quality of life for those living with Parkinson’s.
What are some AI-driven tools for managing Parkinson’s Disease?
AI-driven tools for managing Parkinson’s Disease include wearable devices and apps that monitor symptoms in real-time. These tools collect data on movement, speech, and other indicators, providing insights to healthcare providers for better treatment adjustments. By continuously tracking patient health, AI helps maintain optimal management of the disease.
Can AI help in the early diagnosis of Parkinson’s Disease?
Yes, AI can assist in the early diagnosis of Parkinson’s Disease by analyzing complex data from brain scans and other medical tests. Advanced algorithms detect subtle changes and patterns that might be missed by human eyes. Early diagnosis through AI can lead to earlier intervention, potentially slowing the disease’s progression.
What are the benefits of using AI in Parkinson’s Disease care?
The benefits of using AI in Parkinson’s Disease care include more accurate diagnoses, personalized treatment plans, and continuous monitoring of symptoms. AI helps healthcare providers make data-driven decisions, enhancing the overall effectiveness of care. Additionally, AI can reduce the burden on patients by automating routine tasks and providing real-time support.
How does AI improve medication management for Parkinson’s Disease?
AI improves medication management for Parkinson’s Disease by analyzing patient responses to different treatments and adjusting dosages accordingly. Machine learning algorithms can predict the most effective medication combinations and schedules, reducing side effects and improving symptom control. This personalized approach ensures that patients receive the most appropriate and effective treatment.
What role do wearable devices play in AI-driven Parkinson’s Disease care?
Wearable devices play a crucial role in AI-driven Parkinson’s Disease care by continuously monitoring patients’ movements, tremors, and other symptoms. These devices collect real-time data that AI algorithms analyze to track disease progression and treatment efficacy. The insights gained help doctors adjust therapies promptly, ensuring better management of the condition.
Are there any AI-based therapies for Parkinson’s Disease?
AI-based therapies for Parkinson’s Disease include robotic-assisted physical therapy and cognitive training programs. These therapies use AI to tailor exercises and activities to individual patient needs, enhancing rehabilitation outcomes. AI also helps in optimizing therapy sessions by adjusting intensity and duration based on real-time patient performance and feedback.
What are the challenges of using AI in Parkinson’s Disease treatment?
Challenges of using AI in Parkinson’s Disease treatment include ensuring data privacy and security, integrating AI tools with existing healthcare systems, and obtaining accurate and comprehensive data for AI training. Additionally, there can be resistance to adopting new technologies among healthcare providers and patients. Overcoming these challenges requires collaboration between technologists, clinicians, and policymakers.
How can AI assist in monitoring the progression of Parkinson’s Disease?
AI assists in monitoring the progression of Parkinson’s Disease by analyzing continuous data from patients, such as motor function, speech patterns, and daily activity levels. Advanced algorithms detect subtle changes and trends over time, providing early warnings of disease progression. This allows healthcare providers to adjust treatment plans proactively, maintaining better control over the disease.
What is the impact of AI on Parkinson’s Disease research?
AI has a significant impact on Parkinson’s Disease research by accelerating the analysis of large datasets, identifying potential biomarkers, and uncovering new insights into the disease mechanisms. Machine learning models can process vast amounts of genetic, imaging, and clinical data, leading to more rapid and precise discoveries. This advances our understanding and paves the way for innovative treatments and therapies.
How does AI support caregivers of Parkinson’s Disease patients?
AI supports caregivers of Parkinson’s Disease patients by providing tools that help monitor symptoms, manage medications, and schedule activities. AI-driven applications offer reminders, track patient health, and even predict when symptoms might worsen, giving caregivers valuable insights and reducing their burden. This support system enhances the overall care and well-being of both patients and caregivers.
Can AI predict Parkinson’s Disease flare-ups?
Yes, AI can predict Parkinson’s Disease flare-ups by analyzing patterns in patients’ symptoms and external factors such as stress levels, sleep quality, and medication adherence. By recognizing these patterns, AI algorithms can forecast potential exacerbations, allowing patients and healthcare providers to take preventative measures. This predictive capability helps in maintaining a more stable condition and improving quality of life.
How does AI enhance patient engagement in Parkinson’s Disease management?
AI enhances patient engagement in Parkinson’s Disease management by providing interactive tools and personalized feedback. Mobile apps and virtual assistants can remind patients to take their medication, perform exercises, and track their symptoms. By making disease management more accessible and engaging, AI helps patients take an active role in their own care.
Are there any AI-based diagnostic tools for Parkinson’s Disease?
Yes, AI-based diagnostic tools for Parkinson’s Disease include advanced imaging analysis and voice recognition software. These tools use machine learning to detect early signs of the disease from brain scans, voice patterns, and other biomarkers. Early and accurate diagnosis through AI can lead to more effective treatment plans and better patient outcomes.
What ethical considerations arise from using AI in Parkinson’s Disease care?
Ethical considerations in using AI for Parkinson’s Disease care include patient privacy, data security, and the potential for algorithmic bias. Ensuring that AI systems are transparent and fair is crucial, as well as obtaining informed consent from patients for data usage. Balancing innovation with ethical responsibility is essential to maintain trust and integrity in healthcare.
How is AI being used in clinical trials for Parkinson’s Disease?
AI is being used in clinical trials for Parkinson’s Disease to identify suitable candidates, monitor patient adherence, and analyze trial data more efficiently. AI algorithms can sift through vast amounts of data to find patterns and outcomes that might be missed by traditional methods. This accelerates the research process and helps bring new treatments to market faster.
What future advancements in AI could impact Parkinson’s Disease treatment?
Future advancements in AI could impact Parkinson’s Disease treatment through the development of more sophisticated predictive models, improved wearable technology, and enhanced telemedicine capabilities. AI-driven research might also uncover new therapeutic targets and lead to the creation of personalized medicine based on genetic and molecular profiles. These innovations hold the potential to revolutionize the way Parkinson’s Disease is understood and managed.
How can AI help in managing non-motor symptoms of Parkinson’s Disease?
AI can help in managing non-motor symptoms of Parkinson’s Disease by tracking and analyzing data related to mood, cognitive function, sleep patterns, and autonomic functions. AI-driven tools can provide personalized recommendations and interventions to address these symptoms, improving overall patient well-being. By offering a comprehensive approach, AI supports the holistic management of Parkinson’s Disease.
What role does AI play in rehabilitation for Parkinson’s Disease patients?
AI plays a significant role in rehabilitation for Parkinson’s Disease patients by providing customized exercise programs and real-time feedback. AI-powered rehabilitation devices and apps can adjust exercises based on patient performance and progress, ensuring that therapy is both effective and engaging. This personalized approach helps improve motor skills and functional independence.
How are AI-powered virtual assistants helping Parkinson’s Disease patients?
AI-powered virtual assistants help Parkinson’s Disease patients by offering reminders for medication, appointments, and daily activities. These assistants can also provide information about symptoms and treatments, and offer support for managing daily tasks. By providing constant and accessible support, virtual assistants enhance the quality of life for patients.
Can AI predict the risk of developing Parkinson’s Disease?
AI can predict the risk of developing Parkinson’s Disease by analyzing genetic, environmental, and lifestyle factors. Machine learning models can identify individuals at higher risk by detecting patterns and correlations in large datasets. Early identification of at-risk individuals allows for preventive measures and closer monitoring, potentially delaying the onset of the disease.
How does AI facilitate personalized treatment plans for Parkinson’s Disease?
AI facilitates personalized treatment plans for Parkinson’s Disease by analyzing patient-specific data, including genetic information, symptom patterns, and responses to previous treatments. AI algorithms can suggest tailored therapy options and adjustments, optimizing treatment efficacy. This personalized approach ensures that each patient receives the most suitable care based on their unique needs.
Further Sources
- National Institute of Neurological Disorders and Stroke (NINDS): This institute’s website provides comprehensive information on Parkinson’s disease and various treatment options.
- Michael J. Fox Foundation: This foundation is a key source for research and information on Parkinson’s disease. It also offers resources for patients and caregivers.
- Parkinson’s Foundation: Another organization providing information and support for individuals with Parkinson’s and their families. It offers information on treatment options as well.
- PubMed: A database of medical literature where you can find scientific articles on various treatment approaches for Parkinson’s disease.
- Neurology Journals: Search reputable neurological journals such as “Movement Disorders,” “Neurology,” and “Journal of Parkinson’s Disease” for current research findings and treatment methods.
- Books on Parkinson’s and Neurology: There are many books available on Parkinson’s disease and its treatment, catering to both professionals and laypeople. They could provide valuable information and insights.