
What Are BCIs and Why Are They Gaining Attention in Mental Health?
Technology can literally change how your brain functions. Brain-Computer Interfaces (BCIs) might sound futuristic, but they’re quickly becoming a reality, especially in the field of mental health.
Essentially, BCIs are devices that allow direct communication between the brain and external computers or devices. By harnessing neural stimulation, these systems can alter brain activity, helping to treat a range of conditions, including depression and anxiety.
But why are BCIs grabbing headlines in the mental health space now? The surge of interest is due to advances in neuroscience and technology that allow for more precise interaction with the brain. This is no longer the realm of science fiction. Instead of relying solely on traditional methods like therapy or medication, BCIs offer a fresh approach, addressing the root causes of mental health issues by targeting brain circuits directly.
The Science Behind Neural Stimulation for Mental Health Disorders
The brain is an intricate network of electrical signals. Depression and anxiety disrupt these signals, creating imbalances that traditional treatments may struggle to correct. BCIs, through neural stimulation, aim to reset these imbalances by stimulating specific areas of the brain. Think of it as a “reset button” for troubled minds.
In deep brain stimulation (DBS), for example, electrodes are implanted in the brain to deliver targeted pulses. This method is already showing promise in alleviating depressive symptoms where other treatments have failed. Meanwhile, transcranial magnetic stimulation (TMS) uses electromagnetic fields to non-invasively stimulate nerve cells, offering another less invasive avenue for mental health treatment.
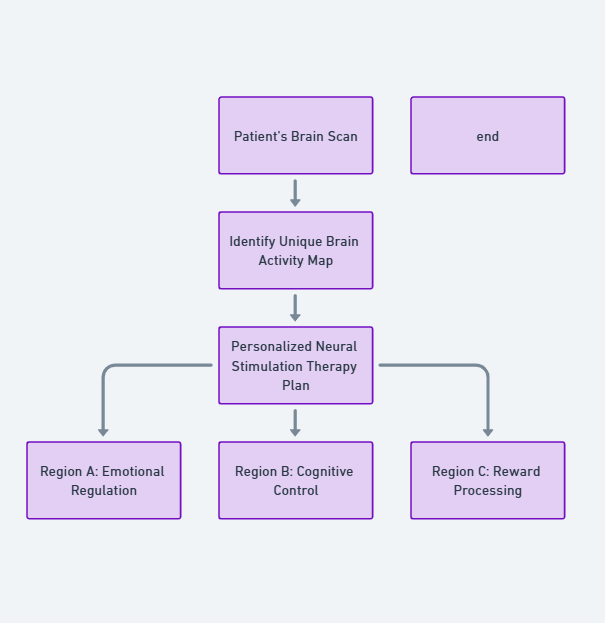
Researchers are excited about the potential to combine brain mapping with BCIs to personalize treatment for each patient. By identifying exactly which neural circuits are malfunctioning, BCIs can deliver customized therapy.
Can Brain-Computer Interfaces Really Treat Depression?
BCIs hold immense potential for treating depression, particularly in patients with treatment-resistant depression. For those who have tried multiple medications, therapies, and lifestyle changes with little success, BCIs offer a new lifeline.
While the science is still evolving, early clinical trials are providing hope. Some patients have experienced significant reductions in depressive symptoms after undergoing BCI treatments, with results that last longer than those from medication. It’s a potential game-changer for those struggling with long-term mental health issues.
How BCIs Alleviate Anxiety Symptoms: A Closer Look
Anxiety disorders are some of the most common mental health conditions worldwide, and BCIs could offer relief where cognitive behavioral therapy (CBT) and medication alone fall short. For anxiety, BCIs target the brain circuits responsible for fear responses and stress regulation. By stimulating areas like the amygdala or anterior cingulate cortex, BCIs may help recalibrate the brain’s stress response, reducing feelings of constant worry or panic.
Interestingly, many individuals report feeling calmer almost immediately after a session of TMS or neurofeedback—a form of BCI therapy where patients learn to regulate their brain activity in real-time. While it’s not a cure-all, the technology provides another layer of treatment, particularly for those who experience persistent anxiety despite traditional approaches.
Personalized Brain-Computer Treatments for Targeted Therapy
One of the most exciting prospects of BCIs in mental health is their potential for personalization. No two brains are exactly alike, which means no two people with depression or anxiety experience the same symptoms or respond identically to treatments. By mapping a person’s unique brain activity, BCIs can be programmed to deliver targeted neural stimulation to the exact areas causing the problem.
This level of precision makes BCIs an exciting tool for customized mental health care. Instead of a one-size-fits-all approach, patients could receive treatment designed specifically for them—whether that’s targeting the circuits responsible for mood regulation or calming overactive stress pathways. This could revolutionize the way we approach mental health, moving from generalized treatments to individualized brain therapy.
Neural stimulation works by modulating brain activity in regions associated with mood regulation, such as the prefrontal cortex. This area of the brain often shows reduced activity in individuals with depression. By stimulating it, BCIs may help “jumpstart” these areas, boosting mood and emotional regulation.
Real-Life Success Stories: BCIs Transforming Mental Health Care
If you’re wondering how all this works in real life, there are already several success stories highlighting how Brain-Computer Interfaces (BCIs) are changing lives. Take the case of a woman who had battled treatment-resistant depression for over a decade. After undergoing deep brain stimulation (DBS), her depressive symptoms drastically reduced within weeks. She described the experience as if a heavy fog had lifted from her mind—a powerful testament to the potential of neural stimulation.

Another individual suffering from severe generalized anxiety disorder (GAD) found relief through transcranial magnetic stimulation (TMS). Traditional treatments failed him for years, but after several sessions of TMS, he noticed that his overwhelming anxiety began to subside, allowing him to resume a more balanced life.
These stories are just the beginning. With BCIs still in their early stages for mental health, more breakthroughs are sure to follow. What’s remarkable is the immediate and long-lasting effects some patients are experiencing—effects that medication and therapy couldn’t deliver.
Bridging the Gap: BCIs as a Supplement to Traditional Therapies
Despite the excitement, it’s important to remember that BCIs are not a replacement for traditional mental health treatments. Instead, they can complement existing therapies, forming a more comprehensive care plan. Many patients undergoing BCI treatments continue to work with their therapists, using BCIs to enhance the effectiveness of therapies like cognitive-behavioral therapy (CBT) or psychotherapy.
For instance, someone receiving TMS for depression might notice they’re more receptive to talk therapy after their sessions. That’s because the brain stimulation helps regulate the areas responsible for emotional control, which may make patients more open to the therapeutic process. Similarly, neurofeedback BCIs can help individuals improve their ability to self-regulate emotions, reducing the frequency of panic attacks or depressive episodes in between therapy sessions.
In this sense, BCIs are the bridge—offering patients a multi-faceted approach to healing.
How Do BCIs Compare to Medication for Depression and Anxiety?
For years, antidepressants and anti-anxiety medications have been the go-to treatments for mental health disorders. But how do BCIs stack up against these pharmaceutical solutions? First off, BCIs target neural circuits directly, unlike medications, which often come with a host of side effects and take weeks to show effectiveness.

Neural stimulation, on the other hand, offers a more immediate intervention with minimal side effects. For many, this is a massive advantage—especially those who have tried multiple medications without success or who can’t tolerate the side effects like weight gain, fatigue, or insomnia that often accompany psychiatric drugs.
However, BCIs aren’t a magic bullet. Medications are still effective for a broad spectrum of individuals, particularly for those with mild to moderate depression or anxiety. But for severe or treatment-resistant cases, BCIs may offer a level of relief that medication alone cannot provide.
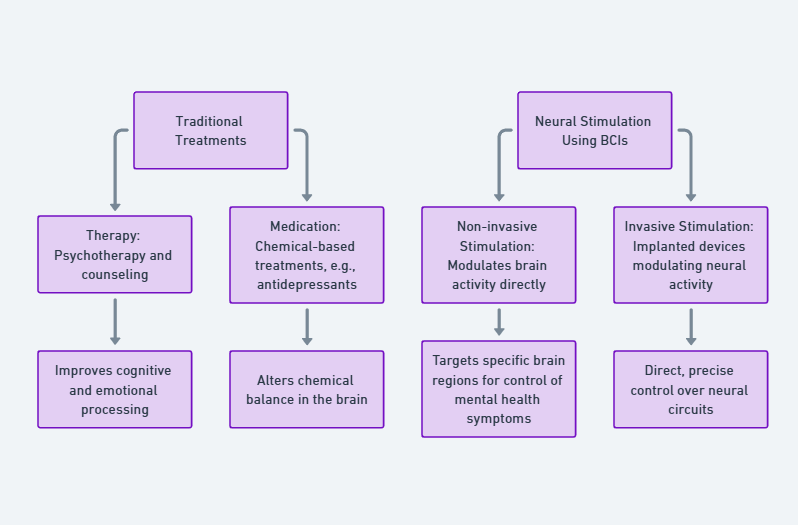
versus neural stimulation using BCIs
The Future of Mental Health: AI-Driven BCIs for Precision Medicine
Looking ahead, the integration of artificial intelligence (AI) with BCIs could be the next big leap in mental health care. Imagine AI algorithms analyzing a patient’s brain activity in real-time, adjusting the level and timing of neural stimulation for maximum effectiveness. This AI-driven personalization could make treatments more precise and dynamic, evolving as the patient’s brain changes over time.
In fact, research is already underway to develop adaptive BCIs that learn from the user’s brain activity and adjust the treatment accordingly. This approach is particularly exciting for chronic conditions, where the brain’s response may shift over the years. By combining neurofeedback, brain mapping, and AI, BCIs could become smarter and more effective with continued use, offering long-term solutions for chronic depression and anxiety.

With this potential on the horizon, it’s easy to imagine a future where BCIs and AI are working hand-in-hand to provide precision medicine for mental health, allowing people to receive care that is truly tailored to their needs.
Challenges and Limitations of Using BCIs in Mental Health Treatments
Of course, BCIs come with their own set of challenges and limitations. For starters, while the technology is promising, it’s still relatively new in the field of mental health. Many of the studies are in their early stages, and long-term effects are not yet fully understood. This means that, while some patients experience incredible results, others may not respond as dramatically—or at all.
Cost is another significant barrier. Brain-Computer Interface treatments, especially invasive procedures like deep brain stimulation (DBS), can be prohibitively expensive. These treatments are often not covered by insurance, making them inaccessible for many who could benefit from them. Even non-invasive treatments like TMS can come with a hefty price tag, limiting widespread use.
Additionally, there are technical hurdles. Not every patient is a good candidate for BCI therapy. Some might have brain patterns that are harder to map or stimulate, which could make the technology less effective for them. There’s also the challenge of fine-tuning the stimulation to the exact areas of the brain causing the issue, as brain circuits are complex and can vary greatly between individuals.
Despite these hurdles, BCIs continue to advance, and with further research and development, these challenges may soon be overcome, paving the way for more affordable and effective mental health treatments.
Are There Risks? Safety Concerns with Neural Stimulation
As with any medical treatment, there are potential risks associated with Brain-Computer Interfaces (BCIs), particularly those involving neural stimulation. One of the primary concerns is invasive procedures like deep brain stimulation (DBS). Since DBS involves implanting electrodes into the brain, there’s always a risk of infection, bleeding, or other surgical complications. Though these risks are relatively low, they are important considerations for anyone contemplating such a treatment.
Even non-invasive methods, like transcranial magnetic stimulation (TMS), come with possible side effects, although they’re generally mild. Some patients report headaches, dizziness, or slight discomfort at the stimulation site. However, these effects are usually short-lived and go away after a few sessions. That said, TMS should be used cautiously in people with a history of seizures, as the stimulation can, in rare cases, trigger a seizure.
There’s also the question of long-term safety. Since BCIs are still relatively new in mental health applications, we don’t yet know the full effects of extended neural stimulation on brain health. Could repeated use cause changes in brain plasticity that lead to unexpected consequences? While current evidence is promising, long-term studies are essential to answer these questions definitively.
Why BCIs Could Be a Game-Changer for Chronic Mental Health Conditions
One of the most exciting possibilities for BCIs is their potential to help individuals with chronic mental health conditions. These are people who have struggled with depression or anxiety for years, often despite trying various treatments without success. For them, BCIs could represent a fresh approach—targeting the brain directly, rather than relying on medications or therapy alone.
The key benefit here is that BCIs are capable of reaching the neural circuits responsible for these chronic conditions. By adjusting activity in areas like the prefrontal cortex or amygdala, BCIs offer a way to regulate mood or anxiety levels with precision. This is particularly appealing for patients with treatment-resistant depression, who often feel like they’ve exhausted all their options.
Moreover, since BCIs provide non-pharmacological interventions, they eliminate the side effects that typically come with long-term medication use, like tolerance, dependency, or unwanted physical effects. For someone managing chronic anxiety, avoiding these side effects while still achieving symptom relief could significantly improve their quality of life.
How Accessible Are BCIs for Everyday Mental Health Treatment?
While the promise of Brain-Computer Interfaces is undeniable, accessibility remains a major hurdle. As mentioned earlier, many BCI treatments—especially invasive ones—are currently expensive and not widely covered by insurance. This limits access to patients with the financial means or those participating in clinical trials.
Non-invasive options like TMS are more affordable but can still be cost-prohibitive for some. The average cost of a TMS session can range from $300 to $500, and multiple sessions are often required to achieve meaningful results. For now, these technologies are mostly available in major medical centers or research institutions, making them less accessible to those living in rural or underserved areas.
That said, as technology improves and demand increases, costs are likely to come down, and access will expand. Telemedicine and remote BCI solutions are also on the horizon, offering potential ways to bring this cutting-edge treatment to a broader audience.
The Road Ahead: What’s Next for BCIs in Treating Mental Illness?
So, what does the future hold for BCIs in mental health care? With advancements in neuroscience, AI integration, and increased understanding of brain function, BCIs are poised to become more effective and accessible in the coming years. Research is continuing at a rapid pace, and newer, less invasive BCI technologies are already in development.
Some experts predict that we’ll soon see home-based BCI systems that allow individuals to monitor and adjust their brain activity from the comfort of their homes. This could be particularly useful for patients managing chronic anxiety or depression, providing them with real-time feedback and instant interventions when they feel symptoms intensifying.
Another exciting area of growth is the combination of virtual reality (VR) and BCIs. By pairing VR with neural stimulation, patients could experience immersive therapy sessions that are not only tailored to their brain’s needs but also enhanced with interactive environments designed to reduce stress or lift mood.
How Public Perception is Shifting Toward BCIs in Mental Health
Public perception of BCIs has evolved significantly. What was once considered science fiction is now seen as a viable option for treating mental health disorders. However, there’s still a level of skepticism and fear, particularly regarding invasive procedures. Concerns about the safety of implanting devices in the brain, as well as fears of losing privacy or control over one’s thoughts, can create hesitation among potential users.
That said, as more success stories emerge and the technology becomes more refined, public confidence is growing. Non-invasive BCIs, like TMS and neurofeedback, have done a lot to dispel some of the fears surrounding brain technology. People are starting to see these devices as tools that enhance mental well-being, rather than invasive machines that control or alter the mind.
As awareness grows, and mental health stigma continues to diminish, it’s likely that BCIs will become a more accepted part of mainstream mental health care—particularly for individuals who haven’t found success with traditional treatments.
Could BCIs Offer Hope for Untreatable Depression Cases?
For many individuals suffering from severe depression, especially those for whom traditional therapies have failed, BCIs could be the breakthrough that brings hope. When medications, therapy, and even lifestyle changes fail, it can feel like the depression is untreatable. BCIs offer an innovative approach by targeting brain regions directly involved in mood regulation.
Neural stimulation doesn’t just mask symptoms—it actively rewires the brain, promoting long-term changes in how emotions are processed. This offers hope, especially for those whose depression has been labeled “treatment-resistant,” and gives a new sense of possibility for recovery when everything else has failed.
As research continues and BCIs become more refined, their potential to bring relief to those who feel they’ve exhausted all options is profound. There’s genuine hope that BCIs will not only complement existing treatments but provide a lifeline for those who have been hardest to treat, offering them a path toward healing and mental well-being.
Conclusion: A New Era for Mental Health Treatment
As we stand at the intersection of neuroscience and technology, Brain-Computer Interfaces (BCIs) represent a powerful new tool for tackling mental health issues like depression and anxiety. From neural stimulation to customized therapies, the potential benefits of BCIs are vast, offering hope to those for whom traditional methods haven’t worked. While challenges like cost, accessibility, and long-term safety still need to be addressed, there’s no denying that BCIs are revolutionizing the mental health landscape.
We’re entering a new era where personalized brain therapy could soon be a reality, providing relief and recovery to millions battling chronic mental health conditions. As technology advances, the possibility of a future where BCIs are as common as therapy or medication seems within reach, offering hope to patients who’ve long been seeking effective solutions. The future of mental health care is not only bright but also incredibly exciting.
Frequently Asked Questions (FAQ)
1. What is a Brain-Computer Interface (BCI)?
A Brain-Computer Interface (BCI) is a technology that creates a direct connection between the brain and an external device, often a computer. BCIs can record brain signals and, in some cases, send feedback to alter brain activity, making them useful for various applications, including mental health treatments.
2. How do BCIs help with depression and anxiety?
BCIs treat depression and anxiety by targeting specific areas of the brain involved in mood regulation and stress response. Through neural stimulation, BCIs can help reset abnormal brain activity, alleviating symptoms. For example, transcranial magnetic stimulation (TMS) uses electromagnetic fields to stimulate areas of the brain that are underactive in people with depression, while neurofeedback helps patients regulate their brain activity in real time.
3. Are BCIs effective for treating treatment-resistant depression?
Yes, BCIs have shown promise in treating treatment-resistant depression, where traditional treatments like medication or therapy fail. In particular, deep brain stimulation (DBS) and TMS have demonstrated success in reducing depressive symptoms in patients who haven’t responded to other therapies.
4. Is BCI treatment painful or uncomfortable?
Most BCI treatments are not painful. Non-invasive BCIs like TMS and neurofeedback cause minimal discomfort, with some patients reporting mild headaches or scalp tingling after TMS sessions. Invasive BCIs, such as DBS, require surgery to implant electrodes in the brain, but these procedures are performed under anesthesia, and discomfort is typically managed post-surgery.
5. How long does it take for BCIs to show results?
The timeline for seeing results with BCI treatment varies. Some patients experience relief after a few TMS sessions, while others may need several weeks or more. In the case of DBS, improvements can take weeks to months as doctors adjust the settings of the implanted device to optimize its effects.
6. Are there side effects associated with BCIs?
BCI treatments are generally safe, but like all medical interventions, they come with potential side effects. For non-invasive BCIs like TMS, side effects may include mild headaches, dizziness, or discomfort at the stimulation site. Invasive BCIs like DBS carry surgical risks, such as infection or bleeding, though these are rare.
7. How do BCIs compare to medications for treating depression and anxiety?
BCIs target neural circuits directly, offering an alternative to medications. While medications can take weeks to work and may cause side effects like weight gain or fatigue, BCIs often provide quicker relief with fewer systemic side effects. However, BCIs are typically considered for patients who do not respond well to medication or for those seeking additional treatment options.
8. Can BCIs be combined with traditional therapies like CBT or medication?
Yes, BCIs can complement traditional therapies such as cognitive-behavioral therapy (CBT) and medications. For example, a person undergoing TMS for depression might also continue with talk therapy, enhancing the benefits of both treatments. Combining BCIs with existing therapies can lead to more comprehensive care.
9. Who is eligible for BCI treatment for mental health?
Eligibility for BCI treatment depends on the individual’s condition and medical history. Non-invasive BCIs like TMS are often recommended for people with depression or anxiety who have not responded to other treatments. Invasive BCIs like DBS are typically reserved for patients with severe, treatment-resistant depression. A mental health professional will assess if a person is a good candidate for BCI therapy.
10. What is the cost of BCI treatment? Is it covered by insurance?
The cost of BCI treatment varies depending on the method. TMS sessions, for instance, can range from $300 to $500 per session, with multiple sessions typically required. DBS, which involves surgery, is more expensive. Insurance coverage for BCIs varies by provider and country, and while some insurers may cover TMS, coverage for DBS or other treatments may be more limited. It’s advisable to check with individual insurance providers for specifics.
11. Are BCIs safe for long-term use?
Current research shows that BCIs are generally safe for long-term use, but as the technology is relatively new, studies are still ongoing to fully understand the long-term effects of continuous neural stimulation. For non-invasive treatments like TMS, there are few known long-term side effects. However, invasive treatments like DBS require regular follow-ups to monitor the device and brain health.
12. How soon will BCIs become widely available for mental health treatment?
BCIs are already available in many major medical centers and research hospitals, especially for treating depression and anxiety. However, wider accessibility, particularly in terms of cost and geographic availability, will likely improve as technology advances and more FDA-approved devices enter the market. Over the next few years, we can expect BCIs to become a more common option in mental health treatment.
13. What’s the future of BCIs for mental health?
The future of BCIs in mental health is bright, with advances in artificial intelligence (AI) promising to make BCI treatments even more personalized and effective. AI-driven BCIs will be able to adjust stimulation in real-time, based on a patient’s brain activity. Home-based BCI devices and virtual reality applications are also being developed, making treatments more accessible and flexible.
Resources
- National Institute of Mental Health (NIMH) – Brain Stimulation Therapies
- Overview of various brain stimulation therapies, including TMS and DBS, commonly used for treating mental health disorders like depression and anxiety.
- NIMH Brain Stimulation Therapies
- American Psychiatric Association – Transcranial Magnetic Stimulation (TMS)
- A detailed explanation of TMS as a treatment for depression, its effectiveness, and how it is administered.
- Nature Neuroscience – Brain-Computer Interfaces for Mental Health
- Scholarly articles on the latest research and advancements in BCIs for the treatment of mental health disorders, covering the neuroscience behind neural stimulation.
- Nature Neuroscience BCIs
- Mayo Clinic – Deep Brain Stimulation (DBS)
- Insights into DBS, including its use for neurological and psychiatric disorders, procedure details, and patient outcomes.
- Mayo Clinic on DBS
- Johns Hopkins Medicine – Neurofeedback and Brain Training
- An introduction to neurofeedback, a non-invasive BCI technology used for training the brain to self-regulate emotions and reduce anxiety symptoms.
- Frontiers in Psychology – BCIs in Psychiatric Care
- A research-based exploration of how BCIs are being integrated into psychiatric care and their potential to revolutionize treatments for depression and anxiety.
- Harvard Medical School – TMS for Depression
- An article explaining how TMS works for treating depression, particularly for patients with treatment-resistant symptoms.
- Harvard on TMS
- World Health Organization (WHO) – Mental Health and Neurological Disorders
- Global insights into mental health trends, the burden of depression and anxiety worldwide, and ongoing efforts to develop technological interventions.
- WHO Mental Health
- Stanford University – Center for Mind, Brain, and Computation
- Research initiatives on brain-computer interfaces and their applications in neural stimulation for treating mental health issues.
- Stanford BCIs
- IEEE Spectrum – The Future of BCIs
- Articles and features on the technological advancements of BCIs, including their medical applications and future potential for treating mental health.
- IEEE Spectrum BCIs
- Mental Health America – Alternative Treatments for Depression and Anxiety
- A consumer guide on emerging alternative treatments, including BCIs, that are gaining traction for treating mental health disorders.
- NeuroTech Reports – Advancements in Brain-Computer Interfaces
- Reports and industry analysis on the latest innovations in BCI technologies, including applications in mental health.
- NeuroTech Reports
- Psychiatric Times – Ethical Considerations of BCIs
- Discussion on the ethical implications of using BCIs for mental health treatment, focusing on patient privacy, consent, and long-term effects.
- Psychiatric Times on BCIs
- The Lancet Psychiatry – BCIs for Treatment-Resistant Depression
- Peer-reviewed studies on the use of BCIs for treating treatment-resistant depression and the impact of neural stimulation on patient outcomes.